Resources
Dr Martin Gale (September 03, 2022) Diagnosis: Fundamental Principles and Methods. Cureus 14(9): e28730. DOI 10.7759/cureus.28730
Abstract posted here with permission of Dr Martin Gale, and under the Creative Commons License Deed Attribution 4.0 International (CC BY 4.0)
Dr Scott Bolland (2016) Neuroscience, AI and the Future of Education TEDxSouthBank
https://www.youtube.com/watch?v=_cYIvfS-knA
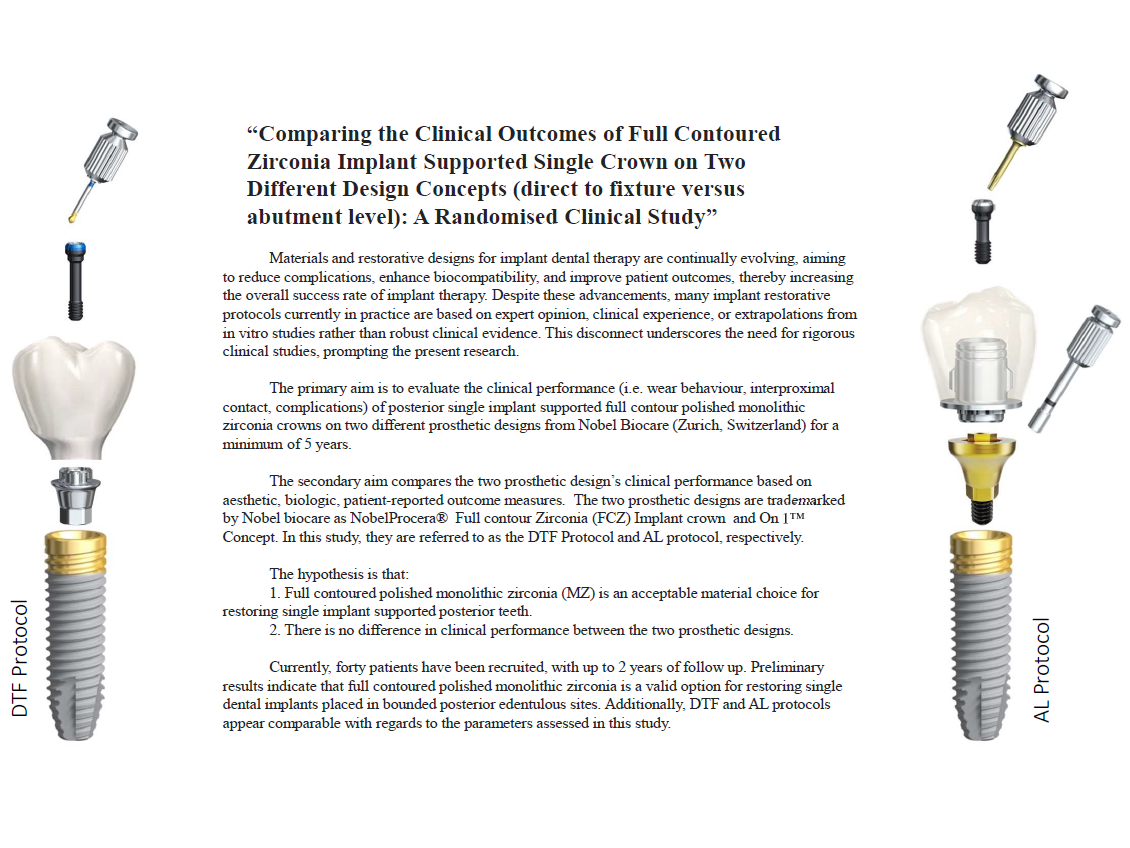
Dr Anny Huang Comparing the Clinical Outcomes of Full Contoured Zirconia Implant Supported Single Crown on Two Different Design Concepts (direct to fixture versus abutment level): A Randomised Clinical Study
Postgraduate Presentation DClinDent(Pros) III University of Melbourne
Dr Cindy Zhou Evaluation of digital and analogue workflows for smile design in prosthodontic planning; an assessment of clinical outcomes and patient satisfaction throughout treatment stages
Postgraduate Presentation DClinDent(Pros) III University of Melbourne
Dr Casey Walsh The influence of scan body design on the accuracy of digital full arch implant scans
Postgraduate Presentation DClinDent(Pros) III University of Queensland
Dr Ken Hooi, Chao Dong, Prof Daniel CN Chan Artificial Intelligence's Role in Dentistry and Teeth Bleaching. American Journal of Dentistry. Accepted for publication 11 July 2024.
Sascha Hein Bridging instrumental and visual perception with improved color difference equations: A multi-center study.
Manuscript abstract posted here with permission of Sascha Hein
Dr Hamza Masood
Angle Correction in Implant Dentistry – A Systematic Review
Retrospective Evaluation of 5–10-year survival and radiographic bone-level changes in single maxillary implant restorations: Dual-Axis versus Uniaxial Dental Implant Analysis
Postgraduate Presentation DClinDent(Pros) III University of Sydney
Dr Casey Walsh
The influence of scan body design on the accuracy of digital full arch implant scans
ABSTRACT
Digital scanning with intraoral scanners has become popular among dental practitioners in prosthodontic treatment due to improved patient-centred outcomes and efficiency when compared to conventional impressions. When used to restore a dental implant, a fiduciary body known as a scan body is required to locate the position of the dental implant within the digital scan and subsequent model. The current body of evidence suggests that digital scans have comparable 3D accuracy to conventional impressions. However, this is based mainly on in vitro studies, and there is a lack of in vivo and clinical studies. The evidence suggests that factors such as intraoral conditions and operator and patient-related factors can negatively influence scan accuracy. Scan body shape, design and material have also been shown to influence the accuracy of digital scans, and designs are highly variable among manufacturers and dental implant systems. There is a lack of published clinical data on the optimal scan body design characteristics to improve the accuracy of digital implant scans, and the currently available in vitro studies show conflicting results. This study aims to evaluate the influence scan body design has on the accuracy of full-arch digital implant scans.
Sascha Hein
Bridging instrumental and visual perception with improved color difference equations: A multi-center study
Abstract
Objectives: This multicenter study aimed to evaluate visual-instrumental agreement of six color measurement devices and optimize three color difference equations using a dataset of visual color differences (∆V) from expert observers.
Methods: A total of 154 expert observers from 16 sites across 5 countries participated, providing visual scaling on 26 sample pairs of artificial teeth using magnitude estimation. Three color difference equations (ΔE*ab, ∆E00, and CAM16-UCS) were tested. Optimization of all three equations was performed using device-specific weights, and the standardized residual sum of squares (STRESS) index was used to evaluate visual-instrumental agreement.
Results: The ΔE*ab formula exhibited STRESS values from 18 to 40, with visual-instrumental agreement between 60% and 82%. The ∆E00 formula showed STRESS values from 26 to 32, representing visual-instrumental agreement of 68% to 74%. CAM16-UCS demonstrated STRESS values from 32 – 39, with visual- instrumental agreement between 61% - 68%. Following optimization, STRESS values decreased for all three formulas, with ΔE’ demonstrating average visual-instrumental agreement of 79% and ∆E00 of 78%. CAM16-UCS showed average visual- instrumental agreement of 76% post optimization.
Significance: Optimization of color difference equations notably improved visual- instrumental agreement, overshadowing device performance. The optimzed ΔE’ formula demonstrated the best overall performance combining computational simplicity with outstanding visual-instrumental agreement.
Dr Hamza Masood
SYSTEMATIC REVIEW
Title:
Angle Correction in Implant Dentistry – A Systematic Review
Abstract:
Objective
This review evaluates success and survival, biological and mechanical complications and patient-related treatment outcomes for dental implants requiring angle correction.
Material & Method
A systematic search in Medline, Scopus, and Google Scholar, alongside manual searches, identified studies meeting inclusion criteria. Sub-crestal and supra-crestal angle correction protocols were included, without restrictions on restorative, surgical, or loading protocols.
Results
Six studies explored sub-crestal angle correction (SAC) via dual axis implants, nine studied angulated screw channels (ASC), and ten assessed angulated abutments (AA). Most studies were prospective or retrospective, with only one randomized controlled trial and one systematic review. Success and survival rates of ≥92% were consistent across all angle correction methods, comparable to conventional implants. Minimal biological and/or mechanical complications, positive functional/aesthetic outcomes, and high patient satisfaction were reported. The degree of angle correction did not significantly impact outcomes. AA showed higher rates of implant failure and increased marginal bone loss.
Conclusion
SAC, ASC, and AA are viable restorative/treatment options providing acceptable functional and aesthetic treatment outcome. Medium term (or short term) treatment outcome showed that AA has been associated with increased mechanical complications, peri-implant bone loss, and implant failure. Long-term prospective studies with larger sample sizes are needed for a definitive understanding of these treatment modalities' success.
RESEARCH
Title:
Retrospective Evaluation of 5–10-year survival and radiographic bone-level changes in single maxillary implant restorations: Dual-Axis versus Uniaxial Dental Implant Analysis
Abstract:
Objective
The objective of this retrospective study is to compare survival rates and radiographic bone-level changes between sub-crestal angle correction (SAC) using 12° dual-axis implants versus conventional uniaxial implants in the maxilla over a period of 5 to 10 years. By analysing patient data and radiographic records, this research aims to evaluate the efficacy and stability of the dual-axis implant design, thereby providing insights into the clinical performance for SAC and compare it to conventional implant restoration.
Material & Method
Patient records were analysed from a single dental practice in Sydney, Australia encompassing the period from 2010 onwards. The inclusion criteria comprised systemically healthy patients who received single external hex implant restorations in the maxilla by the same clinician (K.Y.), with a minimum follow-up period of five years. The primary outcomes assessed were implant survival rates and mesial and distal radiographic bone level changes over the follow-up duration. Radiographic assessments were conducted by two independent examiners (K.Y. and H.M.) in a blinded manner. The Carestream digital dental imaging software was utilised for the analysis. Each radiographic image was calibrated prior to measurement using the implant thread pitch as a reference. Bone levels were measured from the implant platform to the first point of bone-to-implant contact. These measurements were recorded at baseline (time of restoration), and subsequently at 1 year, 3 years, 5 years, 7 years, 9 years, and 10 years post-restoration. The study adhered to standardised protocols for image calibration and measurement to ensure accuracy and consistency.
Results
In progress…….
Conclusion
In progress…….